Pain management strategies
Understanding pain and why strategies matter
Pain management strategies are essential for anyone living with persistent discomfort or facing acute episodes after injury or surgery. Pain is not only a physical sensation. It can affect mood, sleep, relationships and overall quality of life. Clear information about how to reduce pain and restore function helps people make informed choices and improves long term outcomes. This article outlines practical approaches that combine medical care, physical therapy, lifestyle changes and psychological tools so readers can build a sustainable plan for relief.
Types of pain and how they guide strategy selection
Recognizing the type of pain helps determine which pain management strategies work best. Acute pain often follows injury or surgery and typically resolves as tissues heal. Chronic pain persists beyond expected recovery time and may involve ongoing inflammation, nerve changes or pain processing differences in the brain. Nociceptive pain responds well to rest and targeted therapies. Neuropathic pain often needs specific medications and neuromodulation. Mixed pain may require a combination of approaches. Accurate assessment by a qualified provider informs the right mix of therapies.
Core pain management strategies to consider
Effective pain management strategies use multiple modalities together. Combining therapies can reduce reliance on medications while improving function and well being. Core elements include education about pain and pacing activity, structured exercise programs, manual therapies, cognitive and relaxation techniques, sleep improvement, weight management, nutrition and appropriate medication use. When applied in a patient centered way these elements support recovery and long term resilience.
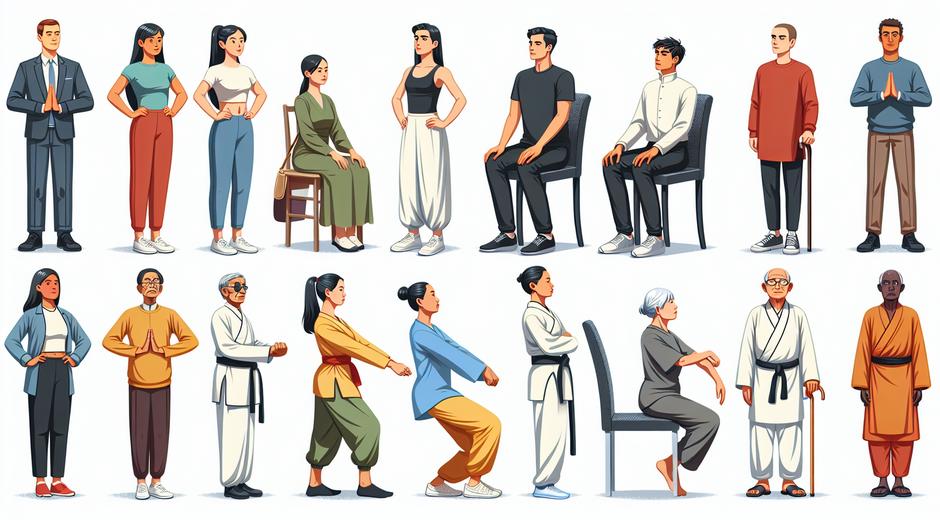
Physical therapies and movement based approaches
Movement is a cornerstone of many pain management strategies. Guided exercise programs designed by physical therapists improve strength, flexibility and joint mobility. Low impact cardiovascular activities such as walking, swimming and cycling increase blood flow and support tissue healing. Manual therapies such as massage and joint mobilization can reduce muscle tension and improve range of motion. For some conditions targeted approaches like pelvic floor therapy or graded motor imagery are highly effective. The key is progressive loading that respects pain limits while gradually expanding capacity.
Mind body approaches that reduce pain perception
Psychological and behavioral strategies change how the brain interprets pain. Cognitive techniques teach patients to reframe unhelpful thoughts about pain and to focus on achievable goals. Mindfulness and meditation practice reduce stress and improve pain tolerance by calming the nervous system. Relaxation training, guided imagery and biofeedback help people recognize and reduce muscle tension and autonomic arousal associated with pain. Social support and group based programs provide validation and practical coping skills that reinforce individual efforts.
Medications and interventional options
Medications remain an important part of many pain management strategies when used thoughtfully. Non opioid analgesics and topical agents are first line for many conditions. Certain neuropathic medications and antidepressant classes can target nerve related pain. Short term use of stronger medications may be indicated after procedures or severe flares. Interventional procedures such as injections, nerve blocks and minimally invasive device therapies are available when conservative care is insufficient. Decisions about medications and procedures should be individualized, weighing benefits, risks and patient goals.
Lifestyle factors that support long term improvement
Lifestyle factors strongly influence outcomes in pain management strategies. Quality sleep is essential for tissue repair and pain regulation. Improving sleep hygiene and addressing sleep disorders can dramatically reduce pain intensity. Nutrition plays a role through inflammation pathways. A balanced diet rich in whole foods, healthy fats and antioxidants supports recovery. Maintaining a healthy weight reduces mechanical stress on joints and the spine. Smoking cessation improves healing and reduces chronic pain severity. Small consistent changes in these areas amplify the effects of clinical treatments.
Developing a personalized pain management plan
There is no single blueprint that fits every person. A personalized plan begins with a thorough assessment that includes medical history, pain characteristics, functioning and personal goals. Collaborating with a care team helps prioritize interventions and set measurable objectives. Short term goals might focus on reducing flare frequency and regaining sleep. Medium term goals can include returning to work or specific daily activities. Long term goals should target sustained function, emotional wellness and prevention of future episodes. Regular review and adjustment are part of effective pain management strategies.
Self management tools and community resources
Empowering individuals with self management tools boosts confidence and reduces reliance on healthcare visits. Pain education programs, home exercise routines and tracking tools increase adherence. Many communities offer pain management workshops and support groups that teach practical strategies and provide encouragement. For additional wellness resources and curated content visit bodywellnessgroup.com which offers guides and articles across categories to support recovery and wellbeing.
When to seek professional help and how to advocate for care
Seek professional help when pain interferes with basic functioning, when new neurological symptoms appear or when pain does not respond to initial self care. A multidisciplinary clinic that includes physicians, physical therapists and mental health providers is ideal for complex cases. Be prepared to describe the pain pattern, what improves and what worsens it, and how it impacts daily life. Ask about evidence based treatments, expected timelines and possible side effects. If conventional options are limited ask about clinical trials or specialized centers that focus on advanced pain management strategies.
Complementary approaches and safe exploration
Some people find benefit from complementary therapies such as acupuncture, cannabis based products when legal and supervised, or certain supplements. It is important to discuss these options with a provider to check for interactions and to ensure safe use. Reliable information sources and quality product selection prevent wasted resources and reduce risk. For curated lifestyle tools and wellness oriented services consider visiting third party resources that collect digital tools and educational content like Moviefil.com which may offer additional support options to complement professional care.
Measuring success and staying adaptable
Success in pain management strategies is not only lower pain scores. It includes improved function, better sleep, reduced medication side effects and enhanced quality of life. Use measurable metrics such as minutes walking per day, days able to work or number of pain flares per month to track progress. Be ready to modify the plan based on outcomes. New evidence and technologies evolve and periodic reassessment ensures the plan remains aligned with personal goals.
Conclusion
Effective pain management strategies combine education, movement, psychological tools, lifestyle changes and medical interventions in a patient centered plan. Collaboration with qualified professionals and consistent self management are key elements. Whether dealing with an acute episode or a long standing condition, focusing on function and quality of life produces meaningful gains. Start with small achievable steps and build a plan that fits personal priorities. For ongoing guidance and wellness resources explore trusted content and local care teams to support your recovery journey.