Vagus Nerve Stimulation: A Complete Guide to Benefits Risks and Clinical Uses
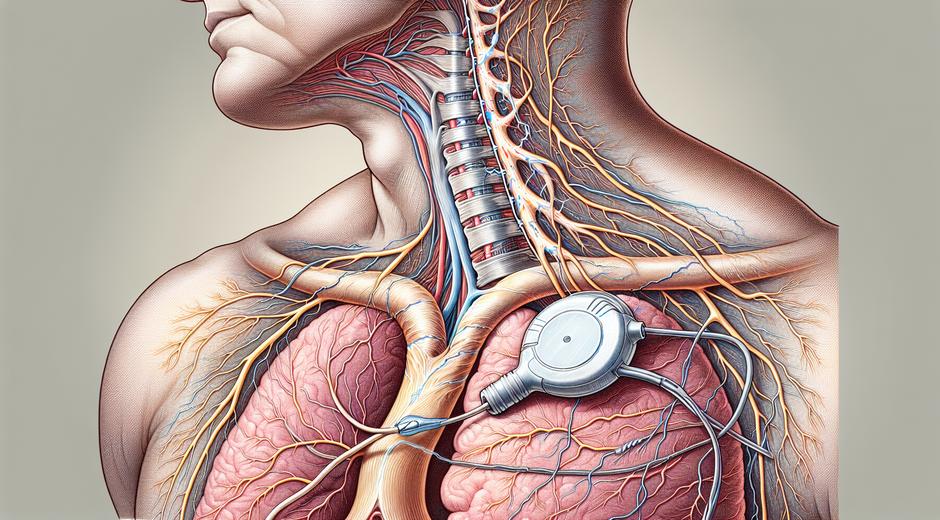
What is Vagus Nerve Stimulation
Vagus Nerve Stimulation is a medical approach that targets the vagus nerve to influence brain and body function. The vagus nerve is the largest cranial nerve and it links the brain to organs such as the heart lungs and digestive tract. By delivering controlled electrical pulses to this nerve clinicians can modulate neural circuits that affect mood pain inflammation heart rate and digestion. Over the last years Vagus Nerve Stimulation has shifted from a niche therapy to a versatile tool in both clinical care and wellness practice.
How Vagus Nerve Stimulation Works
At its core Vagus Nerve Stimulation works by activating the afferent fibers of the vagus nerve. These fibers send signals to key centers in the brain such as the nucleus tractus solitarius the locus coeruleus and the thalamus. Activation of these areas can change neurotransmitter release alter inflammatory signaling and influence autonomic balance. Clinically Vagus Nerve Stimulation is delivered via implanted devices through non invasive devices that use external stimulation or via simple breathing and tone based exercises that stimulate the nerve indirectly.
Types of Vagus Nerve Stimulation
There are several delivery options:
– Implanted devices that provide programmable electrical pulses.
– External devices that use transcutaneous stimulation at the neck or ear.
– Behavioral and breathing techniques that harness the natural biology of the vagus nerve.
Each approach has advantages and limitations that clinicians review when recommending therapy.
Clinical Uses and the Evidence Base
Vagus Nerve Stimulation has evidence for a range of conditions. It is an established treatment for certain types of epilepsy and for treatment resistant depression. Research also suggests benefit in inflammatory disorders such as rheumatoid arthritis and in conditions linked to dysregulated autonomic function such as migraine and cluster headache. Emerging studies explore its role in chronic pain post traumatic stress and metabolic regulation.
Quality clinical trials show measurable improvements in seizure frequency and mood measures for people who receive long term Vagus Nerve Stimulation. For inflammatory conditions early trials show reductions in markers such as C reactive protein and improvements in clinical scores. While evidence is strongest for specific neurological and psychiatric uses ongoing research continues to refine protocols and identify which patients will benefit most.
Benefits of Vagus Nerve Stimulation
Vagus Nerve Stimulation offers several potential benefits:
– Reduction in seizure frequency for selected patients with epilepsy.
– Improvement in mood and reduction in suicidal thinking for treatment resistant depression.
– Decrease in inflammation markers in certain autoimmune conditions.
– Improved heart rate variability which is a marker of better autonomic balance.
– Potential improvement in digestion and gut motility through vagal modulation.
For many patients benefits extend beyond symptom control to improved quality of life and daily function.
Risks and Side Effects
Like any therapy Vagus Nerve Stimulation carries risks. Common side effects from implanted devices include throat discomfort hoarseness cough and changes in voice during stimulation. Surgical risks include infection and device related complications. External stimulation is generally well tolerated with transient skin irritation or mild discomfort. It is important to discuss medical history and any device interactions such as with pacemakers before starting therapy.
Long term monitoring is essential to balance therapeutic benefits and side effects and to make adjustments to stimulation settings.
Who is a Candidate for Vagus Nerve Stimulation
Candidates depend on the condition being treated. For epilepsy and treatment resistant depression patients who have not responded to medications may be evaluated for implanted Vagus Nerve Stimulation. For inflammatory disorders and migraine candidates may try transcutaneous options first. A thorough clinical evaluation includes medical history physical exam and often collaboration between neurology psychiatry and pain specialists.
Patient education is key. Trusted resources and clinic information can help prospective patients learn about options and next steps bodywellnessgroup.com provides curated wellness material that complements clinical guidance.
Home Based Techniques and Self Care
Not all vagal modulation requires devices. Simple practices can enhance vagal tone and support therapy. These include slow diaphragmatic breathing gentle singing or humming exposure to cold water on the face and mindful social connection. These techniques are safe for most people and can be used alongside formal medical treatments. For clinicians educators and students seeking accessible learning tools about nervous system health there are online resources and courses that provide structured information StudySkillUP.com which can help build knowledge for professionals and informed patients.
What to Expect During Medical Treatment
If you proceed with an implanted device you will meet a multidisciplinary team that includes surgeons device specialists and rehabilitation providers. Implantation is performed with a tailored protocol and follow up programming visits help optimize outcomes. For external therapy practitioners typically perform a short training to teach device placement and stimulation parameters. Initial response times vary by condition with some patients noticing early change and others requiring weeks or months of titration.
Ongoing follow up ensures that stimulation settings remain effective and that any side effects are addressed promptly.
Future Directions and Research
Research in Vagus Nerve Stimulation continues to expand. New device designs aim to improve targeting and reduce side effects. Personalized stimulation protocols based on biomarkers may make therapy more precise. Combining Vagus Nerve Stimulation with behavioral approaches pharmacology or neuromodulation from other sites is an area of active study. As data accumulate clinicians will be better positioned to select the right approach for each patient profile.
Practical Considerations and Cost
Access to Vagus Nerve Stimulation varies by region and by health care coverage. Implantable devices have initial surgical costs and ongoing programming visits. External devices may have lower upfront cost and fewer medical requirements. Discussing options with insurance providers and clinic staff can clarify expected expenses and support planning.
Conclusion
Vagus Nerve Stimulation is a versatile therapeutic approach that influences brain body and mind. With evidence supporting its use in epilepsy depression and growing research in inflammatory and pain conditions it represents a meaningful option for many patients. Safety careful selection and thorough monitoring are essential to maximize benefit. Whether you are exploring device based therapy or simple breathing and tone practices enhancing knowledge about vagal function supports better outcomes and informed decision making.
For trusted wellness guidance and lifestyle tools to support nervous system health visit our main site at bodywellnessgroup.com and consider educational resources such as StudySkillUP.com for deeper learning.
Note Consult your health care provider before trying new medical or self care interventions.